A study out in the Endocrine Society's Journal of Clinical Endocrinology & Metabolism has shown that low intake levels of vitamin D during childhood may lead to an increased risk of atherosclerosis approximately 25 years later.
According to the study, 2,148 children aged 3-18 were reexamined at age 30-45. Childhood vitamin D levels were measured from stored serum.
Using the ultrasound technology, carotid IMT (the thickness of the inner layers of the artery) was measured the posterior wall of the left carotid.
Subjects with the lowest vitamin D levels as children had a significantly higher risk of IMT as adults.
Vitamin D and Atherosclerosis
Atherosclerosis is an inflammatory disease in which plaque builds up inside the arteries.
Arteries are responsible for carrying oxygen-enriched blood to the heart and other parts of the body.
Plaque is made up of fat and cholesterol; over time, it hardens and narrows the arteries, thus limiting the flow of oxygen-enriched blood to the heart, organs and other parts of the body.
Therefore, atherosclerosis is the primary cause of cardiovascular disease (Kassi et al, 2013).
Vitamin D deficiency affects 50 percent of the world’s population. It is most known for its role in skeletal and bone health; however, vitamin D deficiency has recently been discovered as a risk factor in heart disease.
Vitamin D receptors are present in all cells associated with atherosclerosis, including the immune cells.
Vitamin D also regulates a wide range of physiological and pathological processes, such as vascular cell growth, migration, and differentiation, immune response modulation, cytokine expression, and inflammatory and fibrotic pathways.
Vitamin D protects against endothelial dysfunction, an inflammatory process that precedes atherosclerosis. Endothelial dysfunction is caused by reduced availability of nitric oxide and increased production of reactive oxygen species.
Vitamin D acts to improve the endothelial nitric oxide synthase coupling, which prevents production and decreases reactive oxygen species production. It also suppresses the enzyme that initiates prostaglandin (PG) catabolism, which suppresses the production of several pro-inflammatory cytokines.
Angiogenesis – a process in which new blood vessels form from pre-existing vessels – is believed to be responsible for the rupture of an unstable atherosclerotic plaque.
Vitamin D inhibits angiogenesis, which is greatly influenced by the migration of ECs. Vitamin D also regulates the expression of profibrotic and antifibrotic factors, considered to be an inflammatory response gene associated with increased risk for thrombosis and atherosclerosis.
Indirect Effects of Vitamin D on Atherosclerosis
In addition to protecting cells against the atherosclerosis process, vitamin D may also protect against systemic conditions that promote atherosclerosis such as insulin resistance, beta-cell dysfunction, dyslipidemia, the renin-angiotensin-aldosterone system (RAAS), and consequent hypertension.
Data suggests that vitamin D protects against insulin resistance, which is associated with endothelial dysfunction, and increased carotid intima-media thickening.
Vitamin D is also able to regulate calcium flux, which aids in insulin secretion that pools in the pancreatic cells. Therefore, vitamin D may improve pancreatic function.
The nutrient furthermore contributes to the proper function of extracellular calcium by ensuring normal calcium influx through cell membranes and by promoting proper insulin intracellular processes, such as phosphorylation of insulin receptors and translocation of glucose transporters (Kassi 2013).
Treating Vitamin D Deficiency in Children
National surveys from the UK, USA and New Zealand show that the prevalence of low vitamin D status among youngsters.
In particular, young children of Asian descent in the UK appeared to be at particular risk of low status compared to similarly aged children of Caucasian origin. This may be due to the increase in skin melanin pigmentation, which can diminish production of vitamin D.
Of potential concern, the prevalence of vitamin D insufficiency in UK adolescents is in excess of 40 percent (Cashman, 2007).
Children can benefit from being exposed to more sunlight during the daytime hours of 11-3 in particular. Vitamin D can be synthesised in the skin and is then metabolised in the liver and kidneys.
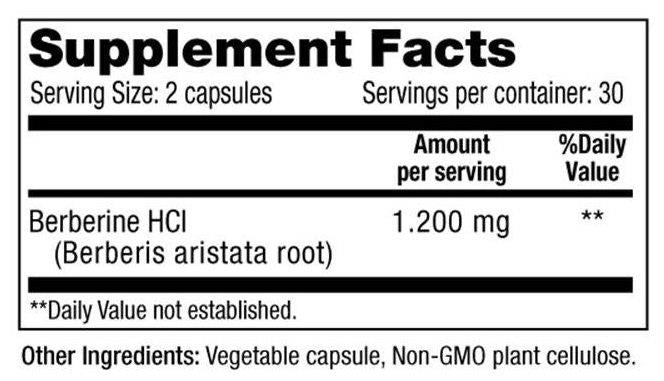
During the winter months, vitamin D can be supplemented through a trusted source. Children who are not able to chew or swallow supplements may benefit from a liquid or powder supplement that can be added to milk, formula or cereal.
The Endocrine Society suggests that infants should have a daily intake of 400 to 1,000 IU (10 to 25 mcg) of vitamin D, and children and adolescents should have a daily intake of 600 to 1,000 IU (15 to 25 mcg) of vitamin D.
Be sure to talk with your child’s paediatrician before starting any supplement regime for your child.
To start supplementing your diet with Vitamin D3, feel free to have a look on our website for more information.
If you're interested in learning about the benefits of vitamin D for children and babies in particular, our in-depth article on the subject is also worth a look.
References
Cashman, K. (2007). Vitamin D In Childhood And Adolescence. Postgraduate Medical Journal, 230-235.
Kassi, E., Adamopoulos, C., Basdra, E., & Papavassiliou, A. (2013). Role of Vitamin D in Atherosclerosis. Circulation, 2517-2531.























Leave a comment